Screening has emerged as a crucial tool in the fight against cancer, enabling the detection of certain tumors months or even years before symptoms prompt a visit to the doctor. In the United States, the U.S. Preventive Services Task Force, a panel of independent medical experts, endorses regular screening for four specific types of cancer: lung, breast, colorectal, and cervical. These recommendations are based on evidence that regular screenings for these cancers can significantly reduce mortality rates without causing undue harm from false positives or unnecessary treatments.
“Screening is on the front lines of reducing deaths from cancer,” stated Robert Smith, an epidemiologist at the American Cancer Society. The task force’s recommendations are periodically reviewed and updated based on the latest scientific evidence, considering factors such as age and potential risk factors, explained Dr. John Wong, vice-chair of the task force. These guidelines are intended for individuals without symptoms, as symptomatic individuals may require different diagnostic approaches regardless of age or screening history.
The Importance of Cancer Screening
The task force’s modeling indicates that regular screening can lead to a 13 percent reduction in lung cancer deaths and a 28 to 30 percent reduction in breast cancer deaths. These figures underscore the life-saving potential of early detection. Furthermore, screening for colorectal and cervical cancers not only facilitates early detection but also plays a role in disease prevention, according to Dr. Smith.
“Beyond finding cancer early, colorectal and cervical cancer screening can also help prevent disease,” Dr. Smith noted.
Understanding the Screening Recommendations
The recommendations for cancer screening are based on a comprehensive review of available evidence. The task force evaluates the benefits and risks associated with screening, aiming to maximize the former while minimizing the latter. This careful balancing act ensures that screenings are both effective and safe for the general population.
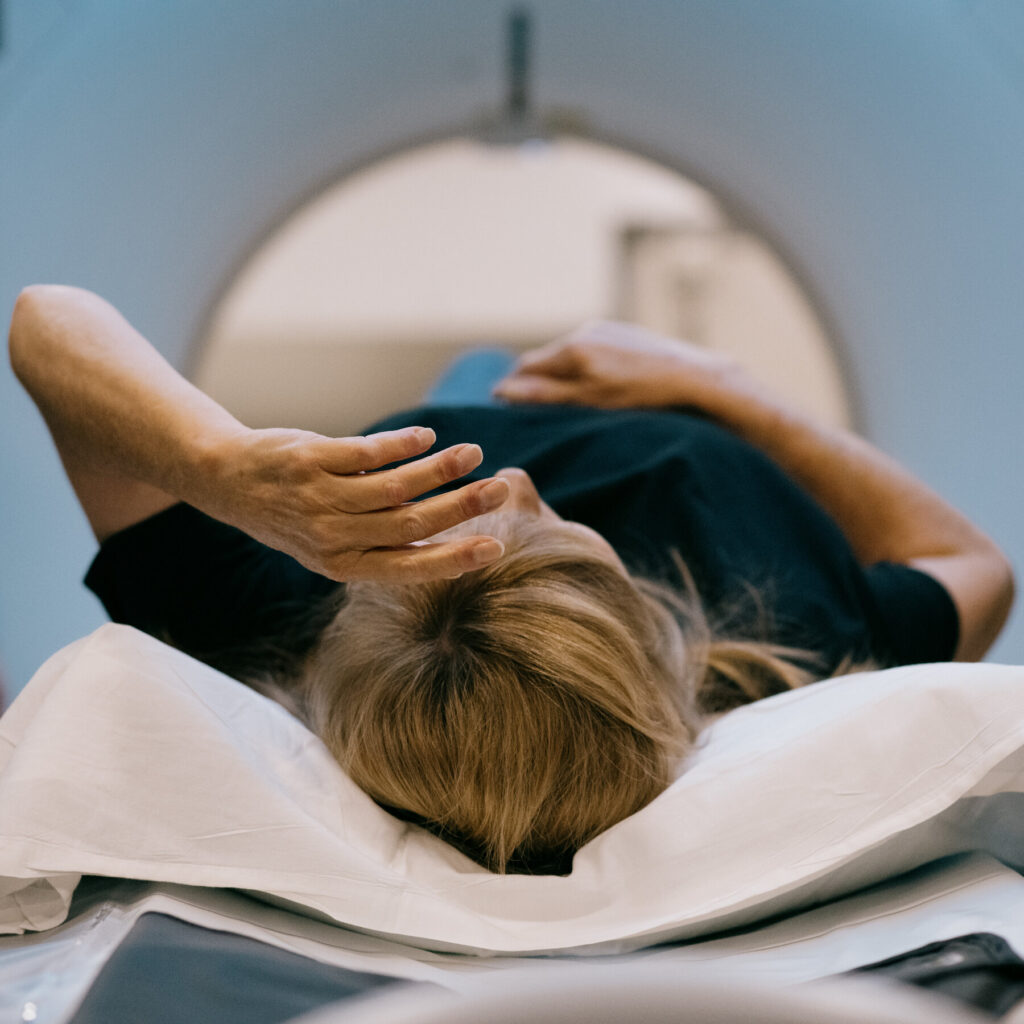
For lung cancer, the task force recommends annual screening with low-dose computed tomography (LDCT) for adults aged 50 to 80 years who have a history of heavy smoking and currently smoke or have quit within the past 15 years. Breast cancer screening is advised for women aged 50 to 74 years, with mammograms every two years. Colorectal cancer screening is recommended for adults aged 45 to 75 years, while cervical cancer screening is advised for women aged 21 to 65 years, with specific guidelines on the frequency and type of tests based on age and health history.
Expert Opinions and Broader Implications
Experts emphasize the importance of personalized screening strategies. Dr. Lisa Richardson, director of the Division of Cancer Prevention and Control at the Centers for Disease Control and Prevention, highlights the need for individuals to discuss their personal risk factors with healthcare providers to tailor screening schedules appropriately. “Understanding your risk and the benefits of screening is key to making informed health decisions,” Dr. Richardson advised.
Meanwhile, the healthcare community continues to explore ways to improve screening technologies and methodologies. Advances in genetic testing and biomarkers hold promise for more precise and individualized screening approaches, potentially expanding the scope of cancers that can be effectively screened.
“The future of cancer screening lies in precision medicine, where we can tailor screenings based on genetic and environmental factors,” Dr. Richardson added.
Looking Ahead: The Future of Cancer Screening
As research progresses, the landscape of cancer screening is likely to evolve. The integration of artificial intelligence in screening processes is already showing potential in enhancing accuracy and efficiency. Moreover, public health initiatives aim to increase awareness and accessibility of screenings, particularly in underserved communities where cancer mortality rates are disproportionately high.
The ongoing challenge remains to balance the benefits of early detection with the risks of overdiagnosis and overtreatment. As Dr. Wong pointed out, “The ultimate goal is to save lives while minimizing harm, and that requires constant vigilance and adaptation to new evidence.”
In conclusion, cancer screening remains a vital component of preventive healthcare. By staying informed about recommendations and engaging in discussions with healthcare providers, individuals can take proactive steps in managing their health and reducing cancer-related risks.
About The Author
 How to Stay Safe During Extreme Summer Heat
How to Stay Safe During Extreme Summer Heat Trump’s Domestic Policy Bill Faces Critical Test in Divided House
Trump’s Domestic Policy Bill Faces Critical Test in Divided House AI Model Revolutionizes Prediction of Sudden Cardiac Arrest Risk
AI Model Revolutionizes Prediction of Sudden Cardiac Arrest Risk Breakthrough Gene Therapy Restores Hearing in Deaf Patients
Breakthrough Gene Therapy Restores Hearing in Deaf Patients Strengthen Your Relationships: Expert Tips for Better Communication
Strengthen Your Relationships: Expert Tips for Better Communication